Suicide prevention in older adults
Here’s my latest article on McKnight’s Long-Term Care News:
Suicide prevention in older adults
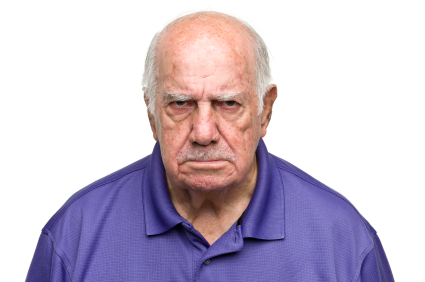
In preparing for a webinar on suicide prevention, I came across startling statistics about suicide rates among older adults. Despite the concern we often hear about teen suicide, the rate for elders is even higher.
While older adults make up 12% of the U.S. population, they account for 18% of all suicide deaths. In 2014, the highest suicide rate in the U.S. population (19.3 per 100,000 people) was among people 85 years or older.
In addition, elder suicide may be under reported by 40% or more. Not counted are “silent suicides,” like deaths from overdoses, self-starvation or dehydration, and “accidents.”
Training staff to assess suicide
Given its prevalence, it’s important for long-term care staff members to know how to recognize and address suicidal thinking and behaviors.
As a psychologist who’s been assessing suicidality since my teen years as a peer counselor in college, I feel comfortable with the process. Most facility staff members, however, haven’t had extensive training and are understandably anxious about an issue that’s likely to be out of their area of expertise. This can lead to over-caution, such as unnecessary one-to-one observation, or to missing signs of distress.
Staff training programs should educate team members about factors increasing the likelihood of depression and thoughts of suicide. Many of these influences are prevalent in our elderly population, such as physical illness, pain, functional impairment, losses and social disconnectedness.
Make use of consulting psychologists by referring residents for evaluation after losses and a decline in condition such as a downgrade in diet from chopped to pureed food, a limb loss, a move from a wheelchair to a reclining chair or a death in the family.
Team communication and support
Virtually all workers know it’s necessary to inform the charge nurse and other personnel about direct statements such as “I want to kill myself,” but staff members should be trained to look for other warning signs of potential suicide, which include changes in grooming, loss of interest in previously appealing activities, giving away possessions and making statements like, “I won’t be needing any more appointments.”
For the entire article, visit:
Suicide prevention in older adults