Category: Customer service
Posted by Dr. El - May 14, 2018 - Customer service, McKnight's Long-Term Care News, Resident care

Here’s my latest article on McKnight’s Long-Term Care News:

You know the scenario: A resident wants to eat donuts, but it will send her blood sugar skyrocketing. The staff members aren’t sure whether to let her indulge as part of person-centered care or to insist on a sugar-free alternative so that they’re not out of compliance with her care plan.
A recent study by Parker et. al examined the staff-perceived conflicts between providing services that are consonant with resident-centered care and those that are in compliance with regulations and the rights of other residents, referred to in their research as “care quality.” They made recommendations based on their findings to ease these conflicts.
The research
They interviewed nursing home staff at 12 different Veterans Administration facilities, including senior leaders, middle managers and direct care staff, asking them questions about care such as, “Is resident-centered care implementation competing with other facility goals?”
All of the nursing homes found some level of conflict between resident-centered care and quality.
The three main areas of divergence were in 1) resident preferences versus medical care, such as issues around dietary compliance, 2) resident preferences and the rights or safety of others, such as someone disrobing in common areas, and 3) “limits on staff ability to respond, related to either time or regulations.”
The first type of conflict was the most common by far, with issues not only around dietary compliance, but also around situations such as when the resident wants to go outside to smoke but weather extremes make it physically unsafe, or residents who are in danger of falling but want to assume the risk and walk unaided.
The second area of friction was related to social or emotional health, such as roommate conflicts. Others related to concerns about physical health, such as when a resident with an infection wants to engage in activities that could put the health of others at risk.
A complicating factor in these instances was the need to explain these situations to family members who might feel that the limits being put on a loved one are not consonant with resident-centered care.
In the third category of conflict, staff members found it difficult to accommodate resident preferences when they were short-staffed, especially at mealtimes when there were multiple demands on their time.
The recommendations
The authors of the study made several recommendations to help minimize these conflicts in the approach to care.
• Determine how each resident feels about the balance of quality of life versus long-term survival. Assess and document the risks involved in their choices and the efforts of team members to mitigate the risks. Helpful tools and examples can be found in this Ideas Institute document, “A Process for Care Planning for Resident Choice.” McKnight’s blogger The Real Nurse Jackie wrote more about the document here.
For the entire article, visit:

Posted by Dr. El - April 27, 2018 - Business Strategies, Customer service, Depression/Mental illness/Substance Abuse, McKnight's Long-Term Care News, Resident care, Role of psychologists, Stress/Crisis management, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

In Editorial Director John O’Connor’s April 16th column, he reported on a study from the Kaiser Family Foundation indicating that increasing numbers of new residents have dementia, are more physically ill and are more likely to be on psychoactive medications.
The study showed that there has been a shift away from long-term services and toward short-term rehab treatment. O’Connor noted the pressure that this puts upon facilities to provide high-quality care in the midst of the churn of residents.
There are many difficulties that can arise from this shift in pace and population, but I’ll focus here on the mental health aspects and their effects on nursing facilities.
One problem that occurs when the length of stay decreases is that the team has a shorter period in which to get to know their residents. They are less likely to notice subtle changes in behavior and mood and they have less time to make the type of personal connection that reassures residents.
Adding to this, the fact that many facilities are operating short of staff in an environment of high employee turnover creates a “perfect storm” of emotional neglect.
Residents enter long-term care facilities in distress. When I adapted the classic Holmes-Rahe Stress Inventory to the circumstances of nursing home admission, I found that residents are experiencing a level of stress considered to be a “life crisis” that puts them at a high risk for further health breakdown. Their families also tend to be in crisis.
Residents and their family members are likely to expect that when they enter long-term care, staff members will provide compassionate medical treatment. Instead, what they frequently find are stressed out nurses and overworked aides who have just enough time to dispense medications or to make up a bed, but none to sit and talk with an understandably anxious resident and their family members about what they can expect regarding their stay and their future.
Social workers — most of whom got into the field in order to provide such counsel — are now buried under a flood of admissions and discharges. They cannot offer emotional sustenance when they need to complete the paperwork on three new admissions and order a walker for the lady whose family wants to take her home tomorrow because her insurance coverage ran out.
It is impossible for direct care staff to provide the same level of service that they did prior to this change in acuity and length of stay. In turn, distress over providing suboptimal care contributes to staff turnover, exacerbating the problem.
For the entire article, visit:

Posted by Dr. El - April 13, 2018 - Business Strategies, Communication, Customer service, End of life, Engaging with families, McKnight's Long-Term Care News, Resident care, Stress/Crisis management, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

In one of the more disturbing encounters I’ve had in long-term care — in a 5-Star deficiency-free nursing home — I offered my condolences to an aide on the loss of a resident she’d cared for over a period of two years.
The aide, a heavyset woman, smiled as she told me that she’d known the resident was dying and had urged the nurse to send her to the hospital quickly. The reason? She didn’t want to wrap the body of the equally heavyset resident after she died.
The resident died among strangers in an ambulance on the way to the hospital.
While I’d like to think the incident was an anomaly, I suspect many if not most nursing homes lack a mission statement for end-of-life care and that most teams can be better prepared for the last months and days of their residents.
Without leadership and training, disorganization and staff priorities can derail the care philosophy of the facility.
Providing decent end-of-life care is more than determining if a resident is DNR or full code. It includes recognizing that someone may be nearing the end of life, referring him or her to hospice while they’re most able to benefit from it, communicating regularly with the resident and their family about their needs, and treating the dying person, their remains and their belongings with respect.
Impact on families
Incidents such as the one above reflect poorly on the organization, even if family members don’t realize that it could have been averted with proper staff training. We often hear how important it is to make a good first impression, but as community institutions relying on reputation and referrals, it’s also essential to make a good last impression.
I’ve heard family members comment that they hadn’t always been pleased with the care at the home but they felt that their mother’s death had been handled with great respect. They left with a feeling of overall satisfaction.
Other families had been reasonably satisfied all along, but departed from the facility in shocked dismay at the end of their parent’s life at the poor communication, insufficient pain management and casual disregard for the belongings of the deceased.
Resident impact
Residents are closely observing how their neighbors’ deaths are handled because they know that this is how they will be treated when their time comes. Based on my experience, the things they find most disturbing are inadequate pain management, unacknowledged deaths and seeing the belongings of their friends removed in clear plastic garbage bags rather than in labeled boxes. They find it most comforting when they see that patients are referred to hospice, surrounded by loved ones, sleeping calmly through the night and when there’s a discussion of the loss among the residents, staff and chaplaincy.
Staff impact
The ways in which facilities handle deaths can have a big impact on staff members as well. As I suggest in “Absenteeism and turnover? Death anxiety could be the cause,” lack of attention to the experience of staff members in handling loss can contribute to employee turnover.
For the entire article, visit:


Posted by Dr. El - March 28, 2018 - Business Strategies, Communication, Customer service, Engaging with families, McKnight's Long-Term Care News, Resident education/Support groups, Technology, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

At Maimonides Medical Center, 24 frail older adults were taught to use laptops so that they could manage their health information from home. The technology facilitated communication between patients and providers and improved the quality of life of participants.
The program was a collaboration between the Department of Geriatrics at Maimonides and the Older Adults Technology Services (OATS), who trained the elders and installed the laptops in their homes. I met with OATS founder Tom Kamber, Ph.D., to follow up on our conversation earlier this year and to hear more about how technology can play a role in reducing costs and improving the quality of care for nursing home residents.
Kamber was enthusiastic about the Maimonides program, noting that the elders, with an average age of 85, were able to use the devices to manage information, communicate with the care team and explore areas of interest.
Fun, he emphasized, is crucial to success.
The desire to connect with the grands on Facebook is a more powerful motivator to learn new skills than is tracking blood sugar levels.
For facilities, particularly those working in healthcare systems focused on providing care at the lowest cost (i.e. in the community or in skilled nursing rather than in the hospital), the ability to remain virtually connected provides a host of benefits. Patients remain within the network, medical issues can be tracked and health crises can be averted before needing expensive hospitalizations. Tailored health information can be offered effortlessly, such as sending out post-surgery information videos at a scheduled time. Patient and family satisfaction increases, as does that of care providers who can quickly answer questions via email rather than return lengthy phone calls at the end of a long workday.
From a mental health standpoint, the program is a winner. Residents and their families are typically anxious about discharge and how to manage once they’re home. A virtual system reduces anxiety because it allows for easy access to medical professionals, offers continuity of care and averts costly, stressful and frequently debilitating hospitalizations.
For the entire article, visit:

Tom Kamber,PhD
Executive Director, OATS
Older Adults Technology Services
Posted by Dr. El - February 15, 2018 - Business Strategies, Customer service, Inspiration, McKnight's Long-Term Care News, Resident care, Tips for gifts, visits

Here’s my latest article on McKnight’s Long-Term Care News:

Last week, I attended an accessible design symposium at the Cooper Hewitt Museum in New York City to see what ideas I could use with elders in long-term care. Through listening to the symposium speakers, reading descriptions of works featured in the student design contest and viewing the Access+Ability exhibit, I found more than I had expected.
Crash course in accessible design
I suspect I’m not the only McKnight’s reader with a lack of knowledge about accessible design — even though we work with elders with abilities that are typically different than those of younger adults.
Patricia Moore, introduced as “the mother of universal design,” told the audience that her elderly grandparents inspired her work. They struggled to maintain their independence in a world that made it difficult for them. “Grandma wasn’t broken,” she said. “The tools we gave her were inadequate.”
In my crash course in accessibility, I learned that objects can be designed in ways that increase the mismatch between our bodies and the environment or, in accessible design, to intentionally decrease that mismatch. For example, the standard design of a walking cane allows it to fall to the floor, making it difficult to retrieve for someone with mobility problems. In the Cooper Hewitt exhibit, I saw canes that stayed upright when not in use.
Another speaker discussed how “designing for disability” very often results in products that are good for everyone, such as books on tape, height adjustable desks or ramps for building access that are used by parents pushing strollers and travelers with rolling suitcases, in addition to those with walkers or wheelchairs.
Nothing about us without us
There was a small, vocal group of disability activists present. When I entered the symposium I was handed a card from their organization that read, “Nothing about us … without us.” They echoed the sentiment of the speakers that increasing the diversity of people designing products and systems results in products and systems that work better for a larger number of people.
Including elders and direct care staff in more of the decisions that affect them within our organizations is likely to result in better decisions.
For the entire article, visit:

Jeweled Hearing Aids

Posted by Dr. El - January 18, 2018 - Communication, Customer service, McKnight's Long-Term Care News

Here’s my latest article on McKnight’s Long-Term Care News:

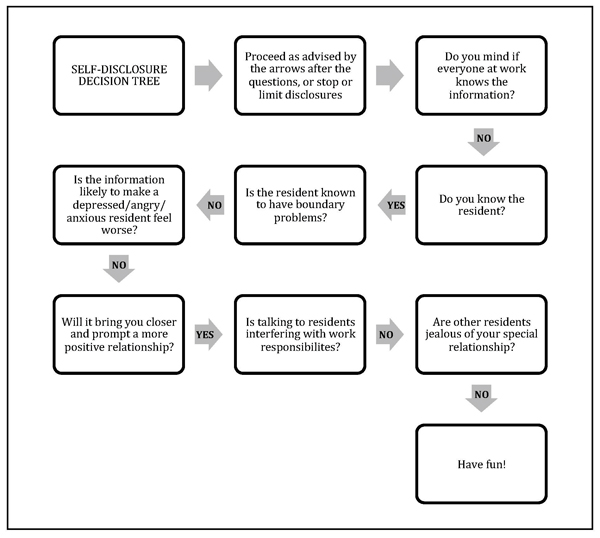
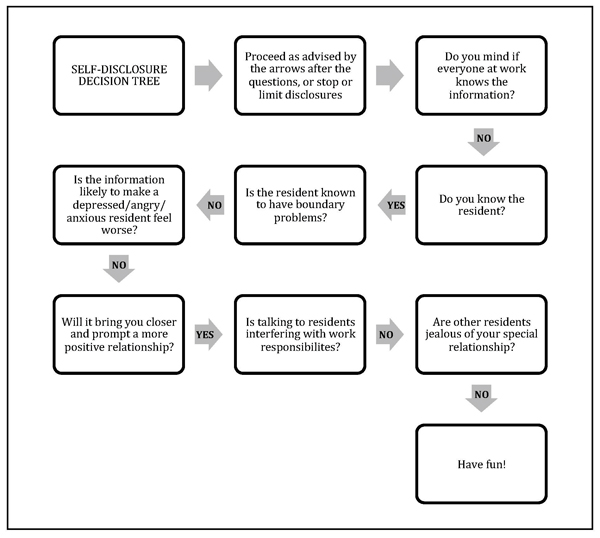
As “Eileen” suggested in the comments section of a recent “Dr. El” blog, disclosing personal information can be a good way to establish a more intimate connection with residents. While self-disclosure can create warmer relationships, there also can be unintended and unwanted consequences to revealing such details.
In contrast to psychologists who study interpersonal interactions for a living, staff members are unlikely to have fully considered the impact of their self-disclosures. Doing so can improve their relationships with residents and avoid unanticipated pitfalls.
Here’s a guide* to the ups and downs of self-disclosure along with a handy flow chart (see below) to help you and your team decide when it’s the right move in any given situation. My inclination toward privacy is reflected in the flow chart, so consider it a starting point for discussion among team members or in a staff training session.
The ups
Part of the pleasure in working with elders is hearing about their lives and learning from their experiences. Sometimes revealing a detail or two from our own lives can help a reticent resident open up.
Self-disclosure allows workers to be more open and relaxed at work and to establish deeper relationships with those in their care.
Being “real” with residents can reduce the somewhat artificial boundaries between people in different phases and roles in their lives and can be part of a healthy organizational culture.
The downs
On the other hand, self-disclosure can sometimes get workers in trouble.
For the entire article, visit:
Posted by Dr. El - November 22, 2017 - Business Strategies, Customer service, McKnight's Long-Term Care News, Motivating staff, Resident care, Something Good About Nursing Homes

Here’s my latest article on McKnight’s Long-Term Care News:

In 2014, I wrote, “I finally visit a Green House (and it blows my mind).” The Green House is designed with a spacious common area, private bedrooms and showers, unobtrusive medical items and universal workers practicing person-centered care. The model shows that it’s possible to make dramatic lifestyle improvements in long-term care.
It seemed that Green Houses were the answer, if only there weren’t so many traditional facilities already in place. Traditional nursing homes can participate in culture change programs with great success if their leadership is committed to the philosophy through the transition period and beyond. They can retrain staff, add plants and pets and remove nursing stations, but the standard long hallways have remained – until now.
Last week I had the opportunity to speak with Rebecca Priest, LNHA, LMSW, Vice President of Skilled Services, at St. John’s Home in Rochester, NY. She’s presiding over one of the most exciting changes in LTC to come down the pike since, well, Green Houses.
St. John’s is taking a conventional nursing home built in the 1960’s with 32 beds to a hall and turning it into 22 small homes modeled after the Green House Project. Each floor is being systematically transformed into homelike environments with a large space for cooking, dining and socializing and universal workers called “Shahbazim” who are central to the model’s success.
Rather than having aides, housekeepers and laundry workers, the Shahbazim do it all. “The Shahbaz role,” Priest says, “is highly skilled and not for everyone. Shahbazim need to collaborate and be part of a highly sophisticated work team.”
Cross-training staff and flattening the work hierarchy reduces the likelihood that workers will find themselves in “systematically disempowered situations where they are set up to fail.” As a resident I knew used to say, “Amen to that!”




Posted by Dr. El - October 25, 2017 - Business Strategies, Customer service, McKnight's Long-Term Care News, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

Long-term care providers have an opportunity to thrive with value-based care, escape cynicism and join the growing wave successful at avoiding readmissions.
Last week, I was part of a panel discussing readmission prevention at the National Readmission Prevention Collaborative’s C-Suite Invitational: New York Transformational Healthcare, which focused on Accountable Care Organizations, bundles and readmissions. The goal of the forum was identifying ways for providers at all ends of the healthcare continuum to prevent hospital readmissions and to thrive in a value-based care model.
Unlike fee-for-service care, which compensates providers for each procedure, value-based care pays for the episode of care, making it essential to coordinate between providers and to avoid unnecessary medical utilization. Efforts to avert hospitalization and readmission are paramount.
The conference offered several takeaways for skilled nursing facilities and other post-acute providers.
From hospital to post-acute provider
Presenters emphasized the importance of being part of a continuing care network rather than a stand-alone facility and of working closely with referral sources. Because crucial information is easily lost during care transitions, best practices suggest a “warm handoff” rather than an exchange of information on paper or via computer, meaning that providers have an actual conversation about care.
To facilitate this, both the referral source, such as the hospital, and the accepting organization, such as the nursing home, should have someone to collect and relay information. To reduce costs, this needn’t be a clinical role as long as the necessary details are conveyed. Communication can be streamlined using a “hotline” between the hospital and the post-acute provider so that phone calls can be made directly rather than routing through the emergency department.
The transition to home
Hospitals are being monitored for readmissions and may have several post-acute care options. The facility most likely to prevent rehospitalization after discharging residents is the one most likely to get referrals.
For the entire article, visit:

Posted by Dr. El - October 12, 2017 - Customer service, McKnight's Long-Term Care News, Resident care

Here’s my latest article on McKnight’s Long-Term Care News:

Perhaps you’ve heard about the administrator who spent a week as a resident in his long-term care facility. After being roused from sleep daily to receive medications that could have been dispensed later in the day, he banned his physicians from unnecessarily prescribing meds during night hours.
That’s an excellent way of attending to sleep hygiene, an important and often overlooked aspect of wellbeing for residents and staff alike.
Sleep challenges of older adults
By the time residents arrive at our doors, their sleep is likely to be affected by influences such as illness and pain. In addition, there are changes in circadian rhythms as people age, leading to increased wakefulness earlier in the morning and fatigue earlier in the evening, according to an article in this month’s American Psychological Association’s Monitor on Psychology.
While we can’t alter some of these factors, as care providers we can become more attuned to the importance of sleep for our residents and train our teams to create environments that are more conducive to slumber.
Impact on care
Poor sleep is associated with cognitive and physical deficits. It can impair residents’ ability to participate in rehab and negatively affect their moods and their interactions with others, including the staff members there to help them (whose job is hard enough).
Residents who can’t sleep through the night due to elements within the control of the facility are not happy with this situation. They’re less satisfied with their stays and therefore less likely to recommend the facility to their friends and neighbors.
As illuminating as it would be, you needn’t sleep in your facility for a week to find out which staff training and policies will remedy the problem. The residents have told me what keeps them up at night and I’ve outlined a “sleep hygiene” training program based on that.
For the entire article, visit:

Posted by Dr. El - September 28, 2017 - Anecdotes, Business Strategies, Communication, Customer service, McKnight's Long-Term Care News, Resident care, Stress/Crisis management

Here’s my latest article on McKnight’s Long-Term Care News:

Both of my mothers-in-law live in long-term care communities in Florida. (I’ll keep the backstory about having two MILs a mystery.)
One MIL lives in a place that was excellent about how they communicated with family members before, during and after Hurricane Irma. The other MIL’s facility handled that aspect of care poorly.
At Bentley Village in Naples on the southwest coast of Florida, all 800 residents of the CCRC were evacuated in advance of the storm, even when everyone thought the hurricane was heading toward the East Coast. While not every organization can afford to evacuate their residents to plush hotels, all of them can afford to do what Bentley did next.
At the top of the home page of its website they placed a bright red banner instructing site visitors to click upon it for more information on Hurricane Irma. The following page contains continually updated reports on the progress the management is making toward assessing and repairing the damage to their homes, as well as an estimate of how long the process will take. A typical entry contains the date and time of the posting, the work that’s been done and what has yet to be accomplished.
They recently added photographs of the damage to the community. The photos clearly show even those most eager to return to their homes why they must wait.
In addition, there’s a list of locations where people are sheltering since residents from skilled nursing, assisted living and independent living were sent to different locales. A pet-friendly hotel was selected for independent living residents with animals.
When I discovered my MIL’s cell phone wasn’t working, I checked the website, got the phone number of the hotel where she was staying and was immediately connected to her room. She claimed they were “having a ball.”
Very reassuring.
For the entire article, visit: