Category: Communication
Posted by Dr. El - March 28, 2018 - Business Strategies, Communication, Customer service, Engaging with families, McKnight's Long-Term Care News, Resident education/Support groups, Technology, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

At Maimonides Medical Center, 24 frail older adults were taught to use laptops so that they could manage their health information from home. The technology facilitated communication between patients and providers and improved the quality of life of participants.
The program was a collaboration between the Department of Geriatrics at Maimonides and the Older Adults Technology Services (OATS), who trained the elders and installed the laptops in their homes. I met with OATS founder Tom Kamber, Ph.D., to follow up on our conversation earlier this year and to hear more about how technology can play a role in reducing costs and improving the quality of care for nursing home residents.
Kamber was enthusiastic about the Maimonides program, noting that the elders, with an average age of 85, were able to use the devices to manage information, communicate with the care team and explore areas of interest.
Fun, he emphasized, is crucial to success.
The desire to connect with the grands on Facebook is a more powerful motivator to learn new skills than is tracking blood sugar levels.
For facilities, particularly those working in healthcare systems focused on providing care at the lowest cost (i.e. in the community or in skilled nursing rather than in the hospital), the ability to remain virtually connected provides a host of benefits. Patients remain within the network, medical issues can be tracked and health crises can be averted before needing expensive hospitalizations. Tailored health information can be offered effortlessly, such as sending out post-surgery information videos at a scheduled time. Patient and family satisfaction increases, as does that of care providers who can quickly answer questions via email rather than return lengthy phone calls at the end of a long workday.
From a mental health standpoint, the program is a winner. Residents and their families are typically anxious about discharge and how to manage once they’re home. A virtual system reduces anxiety because it allows for easy access to medical professionals, offers continuity of care and averts costly, stressful and frequently debilitating hospitalizations.
For the entire article, visit:

Tom Kamber,PhD
Executive Director, OATS
Older Adults Technology Services
Posted by Dr. El - March 3, 2018 - Business Strategies, Communication, McKnight's Long-Term Care News, Motivating staff

Here’s my latest article on McKnight’s Long-Term Care News:

When we think of teamwork in long-term care, we envision a group of dedicated specialists working together to provide the best care for our residents. They read notes from other disciplines, bounce ideas off colleagues at the nursing station and convene care plan meetings.
In reality, teamwork in long-term care is much more complex.
Teamwork basics
Team members include not just clinical staff, residents and family members, but other workers who frequently have an influence on care, including housekeepers, laundry workers, maintenance staff and security guards. To enhance teamwork, these employees should be included in in-service trainings that might initially appear beyond their purview, such as customer service training and education about the medical and behavioral information they may need to relay to the nurses.
Teamwork is strengthened when team members understand the work of their colleagues and when it can best be utilized. For example, a lack of understanding of the difference between psychology and psychiatry services can cause delays in the receipt of needed treatment. Consider monthly training lunches that can boost morale, increase interdepartmental understanding and improve team functioning.
Team members also include those outside the facility, such as medical specialists, dialysis centers and hospitals, as well as consultants who provide onsite care such as psychiatrists, dentists, respiratory therapists and others.
Unifying all these team members requires uncomplicated and reliable conversation and correspondence. Communication can be enhanced in a variety of ways, including computerized records that eliminate paper consults and indecipherable handwriting, enhanced change of shift reports that include behavioral as well as physical information and a management commitment to staff retention to create the stability necessary for a solid team.
Taking it further
Once teamwork basics of role understanding, stable staffing and communication are covered, teams can begin to address teamwork at a deeper level.
Deep teamwork involves observing how the floor, unit or neighborhood is functioning as a whole over different shifts.
A team is not functioning well if a disruptive resident is keeping others awake at night or frightened during the day. Nor is it a high functioning team if two staff members are in a personal argument that’s obvious to all who walk onto the floor.
Deep teamwork calls for observing the interactions of the team and intervening as necessary to guide them back on track.
For the entire article, visit:

Posted by Dr. El - January 18, 2018 - Communication, Customer service, McKnight's Long-Term Care News

Here’s my latest article on McKnight’s Long-Term Care News:

As “Eileen” suggested in the comments section of a recent “Dr. El” blog, disclosing personal information can be a good way to establish a more intimate connection with residents. While self-disclosure can create warmer relationships, there also can be unintended and unwanted consequences to revealing such details.
In contrast to psychologists who study interpersonal interactions for a living, staff members are unlikely to have fully considered the impact of their self-disclosures. Doing so can improve their relationships with residents and avoid unanticipated pitfalls.
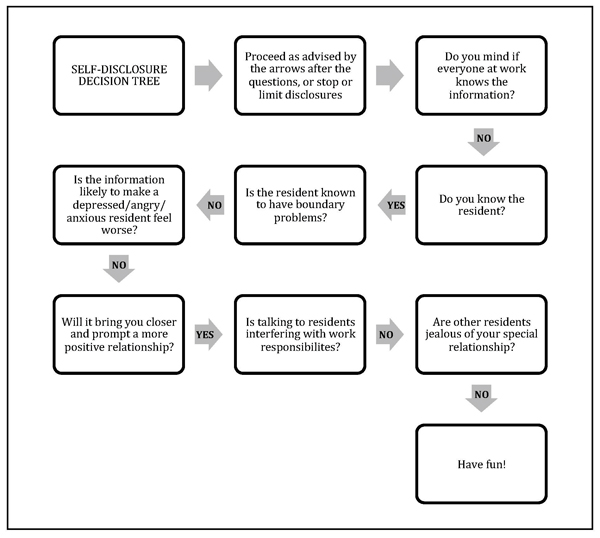
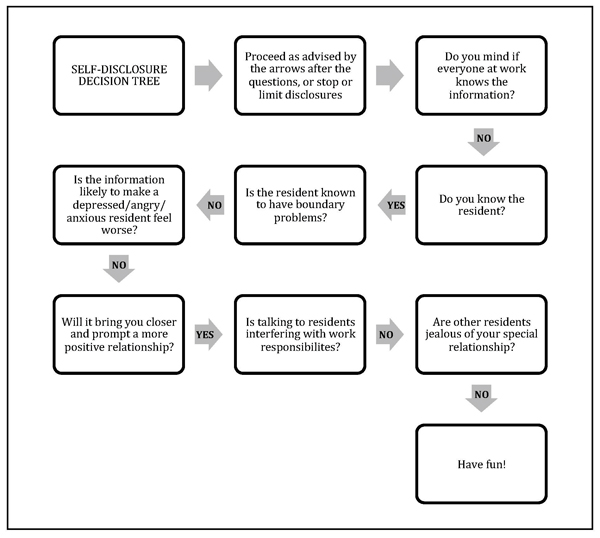
Here’s a guide* to the ups and downs of self-disclosure along with a handy flow chart (see below) to help you and your team decide when it’s the right move in any given situation. My inclination toward privacy is reflected in the flow chart, so consider it a starting point for discussion among team members or in a staff training session.
The ups
Part of the pleasure in working with elders is hearing about their lives and learning from their experiences. Sometimes revealing a detail or two from our own lives can help a reticent resident open up.
Self-disclosure allows workers to be more open and relaxed at work and to establish deeper relationships with those in their care.
Being “real” with residents can reduce the somewhat artificial boundaries between people in different phases and roles in their lives and can be part of a healthy organizational culture.
The downs
On the other hand, self-disclosure can sometimes get workers in trouble.
For the entire article, visit:
Posted by Dr. El - January 4, 2018 - Business Strategies, Communication, McKnight's Long-Term Care News, Motivating staff

Here’s my latest article on McKnight’s Long-Term Care News:

Ahhh. A new year. It’s time for a fresh start, the chance to take life in a different direction.
Many of my friends have remarked to me that they want more focus on family and friends this year. They’d like to achieve a better balance between work and home.
On the job in long-term care, perhaps the goal is to tackle the staff turnover problem or increase profitability. Or maybe the hope is that resident, staff and family satisfaction ratings will be better in 2018 or that this might be the year to achieve a five-star rating.
The common thread between these goals is deepening the attention paid to the people in our personal and business lives.
When staff members don’t feel valued, or inspired by the mission of the company, turnover increases, making it virtually impossible to have high satisfaction scores and five-star ratings. Repeatedly recruiting and training new staff cuts into profit margins and damages worker morale.
To turn things around in one’s personal life, conscious decisions can be made around limiting time on electronics or choosing to fill the new calendar year with events that connect loved ones. At work, changes can occur by prioritizing the way staff members are treated and revamping the culture of the company, altering the way people interact.
Whatever our roles in LTC, there are steps each of us can take to enhance the way we treat each other and to have a positive impact on workplace culture.
• Reevaluate mission and culture. Readers in a position to revise the organizational customs as a whole might enlist experienced guides in the process. A consulting and coaching company such as Drive, with which I’m affiliated, evaluates the strengths and weaknesses of a healthcare organization and provides ongoing support to meet goals throughout the culture change process. As a Drive team member notes in this article onCreating and Sustaining a Strong Culture, follow-through is essential. A consulting team can ensure that bumps in the road don’t become dead ends.
• Investigate known culture change programs. Thankfully, there are many people in our field who have undertaken the daunting task of creating a more gratifying long-term care environment while still following regulations. The new year is an excellent time to take a class with the Pioneer Network or the Eden Alternative, or to learn more about The Green House Model at their 1/9 webinar.
• Promote kindness. If your job in long-term care doesn’t allow you the opportunity to change the overall organizational framework, you can still be an important influence on others with whom you interact by focusing on kindness.

Posted by Dr. El - November 9, 2017 - Business Strategies, Communication, McKnight's Long-Term Care News, Resident education/Support groups, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

Ideas from an interview with Dr. Donna Corrado, Commissioner of the New York City Department for the Aging
Within long-term care, overcoming the problems caused by silos can lead to better care coordination, increased interdepartmental cooperation and reduced work redundancy.
My 1-on-1 interview with Donna Corrado, PhD, Commissioner of the New York City Department for the Aging, suggests there are also benefits to breaking down silos between public and private aging services.
Area Agencies on Aging (AAA)
There are 622 area groups in the National Association Area Agencies on Aging (n4a). According to its website, “the primary mission [of n4a] is to build the capacity of our members so they can help older adults and people with disabilities live with dignity and choices in their homes and communities for as long as possible.”
While n4a’s mission might seem diametrically opposed to the business interests of long-term care, this isn’t the case in a capitated model. When an organization offers a continuum of care with the goal of maintaining people outside of the hospital and at the least expensive level of care, then private and government (and personal) interests align.
My conversation with Dr. Corrado revealed ways of making the most of this alignment of interests, as well as ways to boost the census in long-term care.
AAA offerings
While NYC is the largest Area Agency on Aging in the country, each AAA has it’s own assortment of programs directed toward the needs of their community. There are core issues common everywhere.
Food insecurity is addressed through congregate meals in senior centers and through organizations like Citymeals on Wheels, which provides 8 million meals to New Yorkers Monday through Friday. At the National Readmission Prevention conference I wrote about last month, the speaker from Abbott Nutrition reported that proper nutrition resulted in a 28% decline in hospital readmissions over a six-month period.
Every community has a case management program that assesses individuals and offers home care services.
Senior centers (NYC has 270 of them!) can reduce the epidemic of loneliness and help identify health problems before they become medical emergencies. Funding for senior centers varies greatly, creating opportunities for collaboration.
For the entire article, visit:

Posted by Dr. El - September 28, 2017 - Anecdotes, Business Strategies, Communication, Customer service, McKnight's Long-Term Care News, Resident care, Stress/Crisis management

Here’s my latest article on McKnight’s Long-Term Care News:

Both of my mothers-in-law live in long-term care communities in Florida. (I’ll keep the backstory about having two MILs a mystery.)
One MIL lives in a place that was excellent about how they communicated with family members before, during and after Hurricane Irma. The other MIL’s facility handled that aspect of care poorly.
At Bentley Village in Naples on the southwest coast of Florida, all 800 residents of the CCRC were evacuated in advance of the storm, even when everyone thought the hurricane was heading toward the East Coast. While not every organization can afford to evacuate their residents to plush hotels, all of them can afford to do what Bentley did next.
At the top of the home page of its website they placed a bright red banner instructing site visitors to click upon it for more information on Hurricane Irma. The following page contains continually updated reports on the progress the management is making toward assessing and repairing the damage to their homes, as well as an estimate of how long the process will take. A typical entry contains the date and time of the posting, the work that’s been done and what has yet to be accomplished.
They recently added photographs of the damage to the community. The photos clearly show even those most eager to return to their homes why they must wait.
In addition, there’s a list of locations where people are sheltering since residents from skilled nursing, assisted living and independent living were sent to different locales. A pet-friendly hotel was selected for independent living residents with animals.
When I discovered my MIL’s cell phone wasn’t working, I checked the website, got the phone number of the hotel where she was staying and was immediately connected to her room. She claimed they were “having a ball.”
Very reassuring.
For the entire article, visit:

Posted by Dr. El - September 13, 2017 - Business Strategies, Communication, McKnight's Long-Term Care News, Motivating staff

Here’s my latest article on McKnight’s Long-Term Care News:

I often speak with healthcare groups, giving psychological insights about a variety of issues within long-term care. Sometimes I address a C-suite audience; other times I train direct care staff.
I noticed during the course of these talks that some of the group exercises that generated excitement and intense discussion among direct care staff were met with relative restraint when presented to executives.
After pondering the discrepancy in reactions, I adjusted my talks accordingly and came to this conclusion: Healthcare executives and managers are very different from those they manage.
Understanding and utilizing these differences can facilitate leadership in a variety of ways.
How execs differ from direct care staff
We can consider the discrepancies between the two groups by looking at the traits generally exhibited by each. I’ve borrowed a tool from career counselors, who test their clients’ personality traits to determine what types of jobs best suit them.
One such test is the Myers-Briggs Type Indicator, which examines four different aspects of an individual’s personality as it relates to career choice. The summary below is from an article with a handy chart based on the book, “Do What You Are.”
For the entire article, visit:

Posted by Dr. El - August 31, 2017 - Communication, Customer service, McKnight's Long-Term Care News, Resident care

Here’s my latest article on McKnight’s Long-Term Care News:

By now it’s likely that you, your staff, the residents and their families have seen the incredibly disturbing photo of assisted living residents in Dickinson, TX, sitting in waist-high floodwaters.
Thankfully, all the older women in the picture have been rescued, but that image and others of the flood are undoubtedly causing concern in your community.
Vulnerable residents with no ability to remove themselves from similar situations may be experiencing anxiety, nightmares and/or agitation after seeing their peers immersed in water. Worried family members will want to know that their loved ones are safe from comparable disasters.
Staff members may be wondering what crisis procedures the facility has in place and if they’re sufficiently prepared to carry them out should the need arise (especially with their own families to worry about in an emergency).
Reassurance required
Just as the nation turns to its leaders for reassurance during difficult times, the members of your community will look to you to calm their fears. Now is the time to write a memo to your staff, post a notice in the lobby and add an article to the organization’s newsletter assuring people that there are plans in place for emergencies and that steps have been taken to ensure the safety of the elders entrusted to your care.
Review emergency plans
Review policies and procedures and train staff so that they feel comfortable carrying out these plans. Coordinate with other long-term care facilities so that there is reciprocity of staff and beds in emergency situations.

Posted by Dr. El - June 22, 2017 - Business Strategies, Communication, Engaging with families, Inspiration, McKnight's Long-Term Care News, Something Good About Nursing Homes

Here’s my latest article on McKnight’s Long-Term Care News:

One of the things that most brightens my workday is when I see long-term care residents hanging out together.
In particular, I’ve noticed two ladies who attend activities in tandem wearing dresses with hats and costume jewelry, a threesome of confused residents who sit near the nursing station laughing at jokes only they understand, and an African-American and a Caucasian octogenarian twosome who are amazed to be best friends since neither of them had a friend of the other race before.
Men gather for card games, guys group in the hallway offering wry observations on the behaviors of the staff and other residents, and rehab patients tell me how inspired they are by someone they meet lifting weights in physical therapy. Sometimes I’ll discover that the resident they mentioned is, in turn, inspired by them.
What long-term care offers, aside from medical help and safety, is the opportunity to connect with peers and to maintain a social life. One of our best selling points is the fact that folks can get to activities without needing a coat or umbrella. New residents are often surprised and reassured to learn that there are “transporters” who will bring them to and from daily recreation programs, all for free.
For the entire article, visit:

Posted by Dr. El - June 8, 2017 - Communication, End of life, McKnight's Long-Term Care News, Personal Reflections, Resident care, Stress/Crisis management, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

I waited outside the room until the rehab therapists finished talking to Jim, who’d been admitted to the nursing home the night before. I read over the basic info on his face sheet before my consult. Jim was an 87-year old widower with a long list of diagnoses, some very serious.
After a moment, the rehab people left and I sat across from him and introduced myself and explained my role as the psychologist.
“How are you handling all of this stress?” I asked.
“I’m dying,” he replied.
“You don’t think you’ve got much time left?”
“No.”
“Does that upset you?”
“No, not particularly.”
He seemed quite calm.
“Are you sleeping okay? Eating okay?” I proceeded to ask him all the questions I’m supposed to ask patients I meet for the first time. “What kind of work did you do?”
He quietly answered them all. After a while there was a knock on the door and his physician poked her head into the room. “Just give me a minute. I’ll finish up,” I assured her, and turned back to Jim.
“It’s one of us right after the other, isn’t it?” I commented. “Let’s stop here today and I’ll come back next week to see how you’re doing.”
He gave me a funny look and half-shrugged. The doctor knocked again and I rose to leave.
It wasn’t until I returned to work the following week, when I learned Jim had died, that I realized his look meant, “I told you. I’m dying. I won’t be here next week.”
In hindsight, I wished I’d asked Jim more specifically what he meant when he said he was dying. People sometimes make remarks like that to me in their first few days in the nursing home without meaning that they’re in the active dying process. If I’d realized I wouldn’t have more time with Jim, I would have abandoned my standard questions and focused more on being present with him.
I was even more distressed that Jim had spent his last day fielding interviews from well-meaning staff members determined to provide good care. He was patient and kind about it. I’m guessing he was a really pleasant man, maybe too nice for his own good. That might have been something we could have worked on in psychotherapy.
If I knew I was dying, I wouldn’t want to spend my last day answering the questions of strangers trying to provide services I knew I wouldn’t be around to receive. I hope I’d be more assertive than Jim about refusing care, but there must be a way to offer a better experience for a dying person than having to rely on their level of assertiveness when ill and faced with medical routines. Perhaps we could establish a “last day” protocol.
For the entire article, visit: